Piperacillin/Tazobactam
Emery Haley, PhD, Scientific Writing Specialist
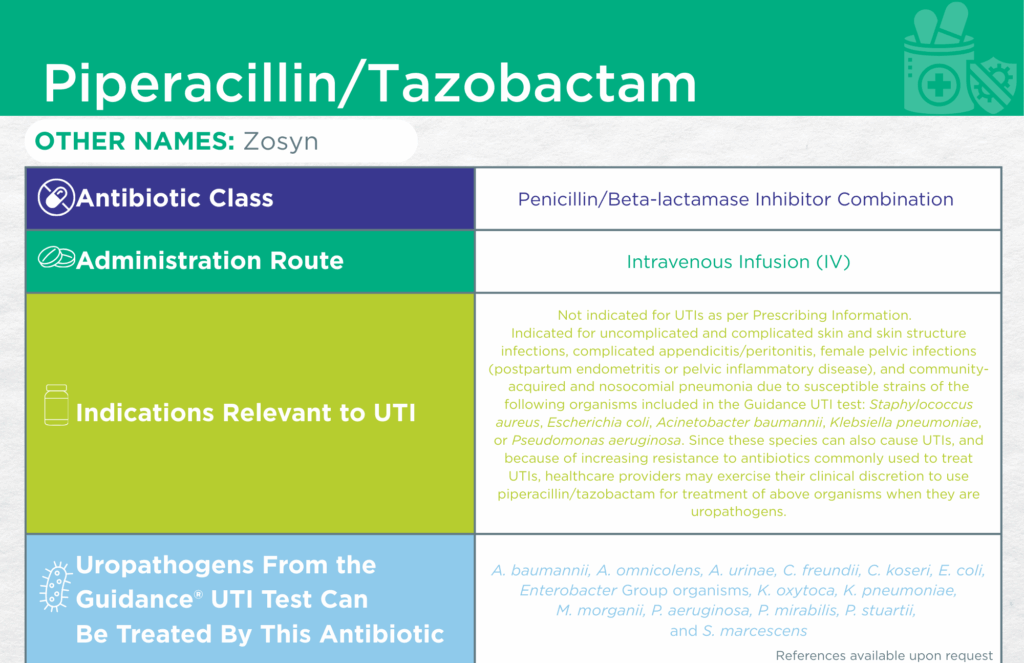
Piperacillin/Tazobactam
Find the Latest FDA-Approved Labelling Information Here: Drugs@FDA Online Database
Administrative Routes
Parenteral [intravenous infusion (IV)]
Other Names
Zosyn
Bacteriostatic or Bactericidal
Bactericidal [1]
Antibiotic Class
Penicillin/Beta-lactamase Inhibitor Combination
Mechanisms of Action
This antibiotic leverages dual mechanisms of action.
Piperacillin, a beta-lactam antibiotic, binds to penicillin-binding proteins (PBPs) on bacterial cell walls. PBPs are essential for the formation of peptidoglycan, which gives the bacterial wall strength and integrity. Binding of piperacillin to PBPs leads to failure of peptidoglycan cell wall synthesis, causing bacterial cell death.
Some bacteria develop resistance to beta-lactam antibiotics, like piperacillin, by producing enzymes, called beta-lactamases, that degrade the antibiotic. Tazobactam helps preserve the activity of beta-lactam antibiotics by inhibiting these enzymes and allowing piperacillin to then bind to PBPs and cause bacterial cell wall degradation.
WHO AWaRe Classification
Watch [2]
Empiric Use Recommendations
Yes (preferred for complicated UTI with or without sepsis) [Infectious Diseases Society of America (IDSA)] [3]
Indication(s) Relevant to UTI
Not indicated for UTIs as per Prescribing Information.
Indicated for uncomplicated and complicated skin and skin structure infections, complicated appendicitis/peritonitis, female pelvic infections (postpartum endometritis or pelvic inflammatory disease), and community-acquired and nosocomial pneumonia due to susceptible strains of the following organisms included in the Guidance® UTI test: Staphylococcus aureus, Escherichia coli, Acinetobacter baumannii, Klebsiella pneumoniae, or Pseudomonas aeruginosa.
Since these species can also cause UTIs, and because of increasing resistance to antibiotics commonly used to treat UTIs, healthcare providers may exercise their clinical discretion to use piperacillin/tazobactam for treatment of above organisms when they are uropathogens.
Checkmarks
CLSI and/or FDA documents support the efficacy of this antibiotic against the following organisms from the Guidance® UTI test: Acinetobacter baumannii, Aerococcus urinae, Citrobacter freundii, Citrobacter koseri, Escherichia coli, Enterobacter Group organisms, Klebsiella oxytoca, Klebsiella pneumoniae, Morganella morganii, Pseudomonas aeruginosa, Proteus mirabilis, Providencia stuartii, and Serratia marcescens.
Published primary literature supports the efficacy of this antibiotic against the following organism from the Guidance® UTI test: Alloscardovia omnicolens [4]
- Ishak, A.; Mazonakis, N.; Spernovasilis, N.; Akinosoglou, K.; Tsioutis, C. Bactericidal versus Bacteriostatic Antibacterials: Clinical Significance, Differences and Synergistic Potential in Clinical Practice. J. Antimicrob. Chemother. 2024, 80, 1–17, doi:10.1093/jac/dkae380
- AWaRe Classification of Antibiotics for Evaluation and Monitoring of Use, 2023 Available online: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2023.04 (accessed on 6 February 2025).
- Complicated Urinary Tract Infections (CUTI): Clinical Guidelines for Treatment and Management Available online: https://www.idsociety.org/practice-guideline/complicated-urinary-tract-infections/ (accessed on 28 July 2025).
- Isnard, C.; Lienhard, R.; Reissier, S.; Rodriguez, S.; Krähenbühl, J.; Liassine, N.; Guérin, F.; Cattoir, V. In Vitro Antimicrobial Susceptibility of Alloscardovia Omnicolens and Molecular Mechanisms of Acquired Resistance. Diagnostic Microbiology and Infectious Disease 2016, 84, 227–229, doi:10.1016/j.diagmicrobio.2015.08.009.
Dr. Emery Haley is a scientific writing specialist with over ten years of experience in translational cell and molecular biology. As both a former laboratory scientist and an experienced science communicator, Dr. Haley is passionate about making complex research clear, approachable, and relevant. Their work has been published in over 10 papers and focuses on bridging the gap between the lab and real-world patient care to help drive better health outcomes.