Sulfamethoxazole/Trimethoprim
Emery Haley, PhD, Scientific Writing Specialist
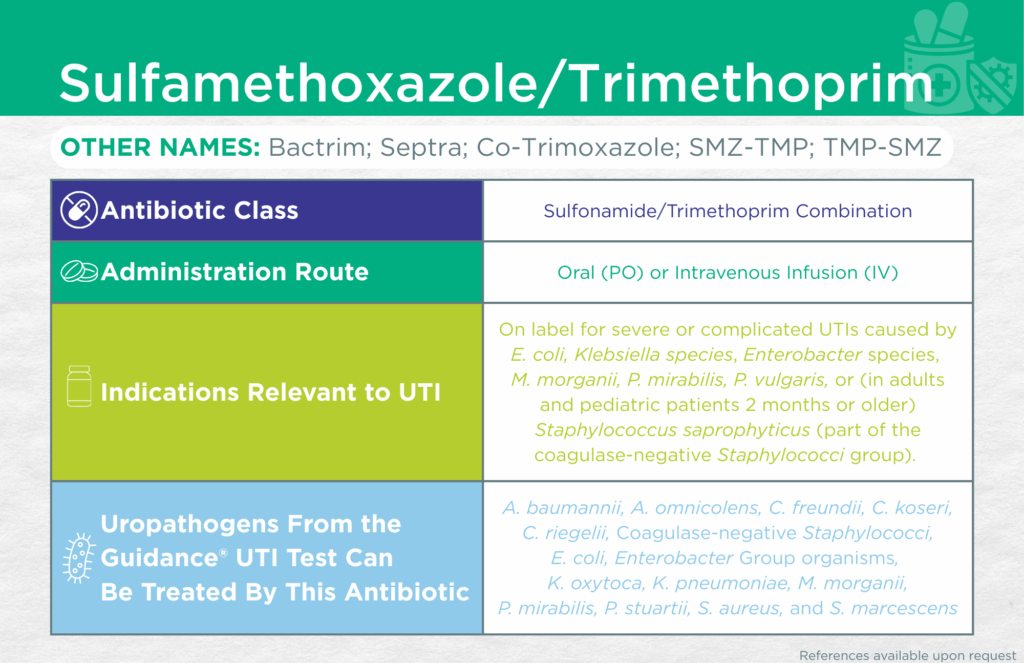
Sulfamethoxazole/Trimethoprim
Find the Latest FDA-Approved Labelling Information Here: Drugs@FDA Online Database
Administrative Routes
Oral (PO) or Parenteral [intravenous infusion (IV)]
Other Names
Bactrim; Septra; Co-Trimoxazole; SMZ-TMP; TMP-SMZ
Bacteriostatic or Bactericidal
Bactericidal (due to the synergistic effects of combining both agents) [1]
Antibiotic Class
Sulfonamide/Trimethoprim Combination
Mechanisms of Action
Sulfamethoxazole is a direct competitor of the bacterial dihydropteroate synthase enzyme. Inhibition prevents the conversion of para-aminobenzoic acid (PABA) to dihydrofolic acid, a step in the creation of the active form of folate. Trimethoprim is a direct competitor of the bacterial dihydrofolate reductase enzyme. Inhibition prevents the conversion of dihydrofolic acid to tetrahydrofolic acid, the active form of folate.
The two agents act synergistically to block bacterial production of bioactive folate, preventing bacterial DNA, RNA, and protein synthesis, resulting in bacterial cell death.
WHO AWaRe Classification
Access [2]
Empiric Use Recommendations
Yes (lower UTI/cystitis) [World Health Organization (WHO), Infectious Diseases Society of America (IDSA)*, and American Urological Association (AUA)] [3-5]
*This recommendation ONLY applies when local antibiograms indicate a resistance rate of < 20% among the likely or confirmed infecting organism(s). Avoid if used by the patient in the previous 3 months for a UTI.
Yes (preferred for complicated UTI without sepsis) [Infectious Diseases Society of America (IDSA)] [6]
Indication(s) Relevant to UTI
On label for treatment of severe or complicated UTIs caused by Escherichia coli, Klebsiella species, Enterobacter species, Morganella morganii, Proteus mirabilis, Proteus vulgaris, or (in adults and pediatric patients 2 months or older) Staphylococcus saprophyticus (part of the coagulase-negative Staphylococci group).
Checkmarks
CLSI and/or FDA documents support the efficacy of this antibiotic against the following organisms from the Guidance® UTI test: Acinetobacter baumannii, Citrobacter freundii, Citrobacter koseri, Corynebacterium riegelii, Coagulase-negative Staphylococci, Escherichia coli, Enterobacter Group organisms, Klebsiella oxytoca, Klebsiella pneumoniae, Morganella morganii, Proteus mirabilis, Providencia stuartii, Staphylococcus aureus, and Serratia marcescens.
Published primary literature supports the efficacy of this antibiotic against the following organisms from the Guidance® UTI test: Alloscardovia omnicolens [7]
- Ishak, A.; Mazonakis, N.; Spernovasilis, N.; Akinosoglou, K.; Tsioutis, C. Bactericidal versus Bacteriostatic Antibacterials: Clinical Significance, Differences and Synergistic Potential in Clinical Practice. J. Antimicrob. Chemother. 2024, 80, 1–17, doi:10.1093/jac/dkae380
- AWaRe Classification of Antibiotics for Evaluation and Monitoring of Use, 2023 Available online: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2023.04 (accessed on 6 February 2025).
- The WHO AWaRe (Access, Watch, Reserve) Antibiotic Book – Infographics – PAHO/WHO | Pan American Health Organization Available online: https://www.paho.org/en/documents/who-aware-access-watch-reserve-antibiotic-book-infographics (accessed on 22 July 2025).
- Gupta, K.; Hooton, T.M.; Naber, K.G.; Wullt, B.; Colgan, R.; Miller, L.G.; Moran, G.J.; Nicolle, L.E.; Raz, R.; Schaeffer, A.J.; et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 2011, 52, e103–e120, doi:10.1093/cid/ciq257.
- Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline (2022) – American Urological Association Available online: https://www.auanet.org/guidelines-and-quality/guidelines/recurrent-uti (accessed on 6 February 2025).
- Complicated Urinary Tract Infections (CUTI): Clinical Guidelines for Treatment and Management Available online: https://www.idsociety.org/practice-guideline/complicated-urinary-tract-infections/ (accessed on 28 July 2025).
- Isnard, C.; Lienhard, R.; Reissier, S.; Rodriguez, S.; Krähenbühl, J.; Liassine, N.; Guérin, F.; Cattoir, V. In Vitro Antimicrobial Susceptibility of Alloscardovia Omnicolens and Molecular Mechanisms of Acquired Resistance. Diagnostic Microbiology and Infectious Disease 2016, 84, 227–229, doi:10.1016/j.diagmicrobio.2015.08.009.
Dr. Emery Haley is a scientific writing specialist with over ten years of experience in translational cell and molecular biology. As both a former laboratory scientist and an experienced science communicator, Dr. Haley is passionate about making complex research clear, approachable, and relevant. Their work has been published in over 10 papers and focuses on bridging the gap between the lab and real-world patient care to help drive better health outcomes.