S. marcescens
Emery Haley, PhD, Scientific Writing Specialist
Serratia marcescens
Clinical Summary
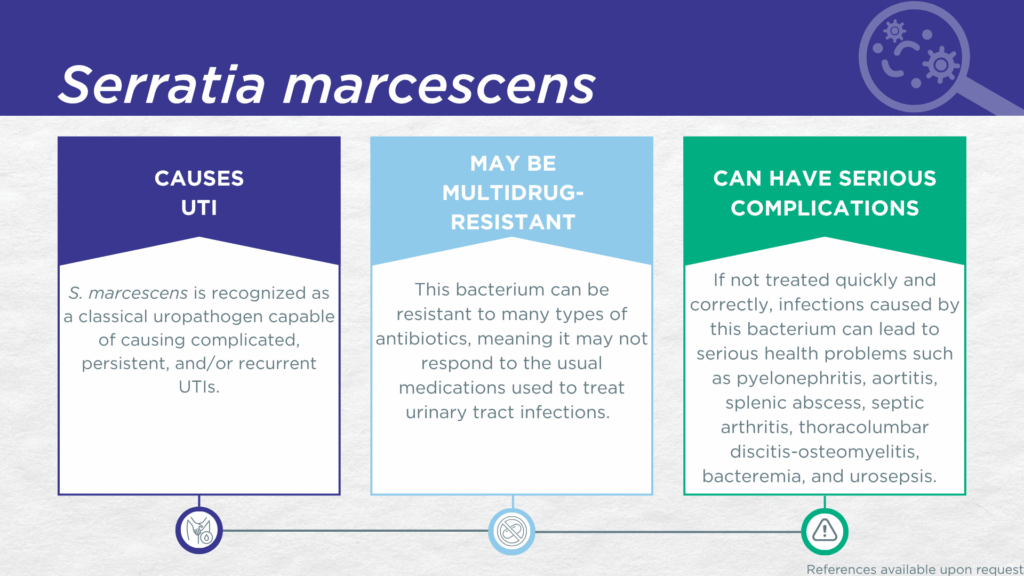
- S. marcescens is recognized as a classical, urease-positive, gram-negative, biofilm-forming, uropathogen.
- S. marcescens is associated with complicated UTI.
- In symptomatic UTI patients, S. marcescens:
- Is not a contaminant (is found in catheter-collected urine specimens).
- Is viable (can grow out on culture).
- Is pathogenic (associated with elevated urine biomarkers of infection).
- Reported severe complications of S. marcescens UTI include pyelonephritis, aortitis, splenic abscess, septic arthritis, thoracolumbar discitis-osteomyelitis, bacteremia, and urosepsis.
- Multidrug-resistant S. marcescens is a significant global health threat.
Bacterial Characteristics
Gram-stain
Gram-negative
Morphology
Bacillus
Growth Requirements
Non-fastidious (grows well in standard urine culture conditions)
Facultative anaerobe
Nitrate Reduction
Yes
Urease
Positive
Biofilm Formation
Yes
Pathogenicity
Colonizer or Pathobiont
Clinical Relevance in UTI
S. marcescens is a biofilm-forming, urease-positive, gram-negative microorganism with some strains producing a red pigment. S. marcescens is commonly recognized as a cause of severe nosocomial infections in high-risk groups including newborns, older adults, immunocompromised individuals, and intensive care patients with invasive medical devices.[1,2] However, S. marcescens is also considered a classical uropathogen, with several known virulence factors and increasing numbers of multidrug-resistant urinary isolates reported.[3–5]
In a study of older adult males and females with clinically suspected complicated UTI, S. marcescens was detected in both midstream voided and in-and-out-catheter collected specimens indicating that it was truly present in the bladder, not simply a contaminant picked up during voiding.[6] Furthermore, elevated markers of immune system activation in the urinary tract have been measured from the same clinical urine specimens in which S. marcescens was detected, indicating that the presence of S. marcescens was associated with an immune response to urinary tract infection.[7–9]
Although not considered one of the six highest priority “ESKAPE” pathogens, the World Health Organization (WHO) has included third-generation-cephalosporin-resistant and carbapenem-resistant Enterobacterales, including S. marcescens, in the “critical” group of the 2024 Bacterial Priority Pathogens List (BPPL).[111] Severe complications of S. marcescens UTI, including pyelonephritis, aortitis, splenic abscess, septic arthritis, thoracolumbar discitis-osteomyelitis, bacteremia, and urosepsis, have been reported.[10,11]
Together, these findings indicate that S. marcescens should be seriously considered as a uropathogen and demonstrate the value of detecting this organism, particularly in individuals with risk factors for complicated UTI.
Treatment
Evidence of Efficacy (Checkmarks): Cefepime, Ciprofloxacin, Doxycycline, Gentamicin, Levofloxacin, Meropenem, Piperacillin/Tazobactam, Sulfamethoxazole/Trimethoprim, and Trimethoprim.
- Cosimato, I.; Santella, B.; Rufolo, S.; Sabatini, P.; Galdiero, M.; Capunzo, M.; Boccia, G.; Folliero, V.; Franci, G. Current Epidemiological Status and Antibiotic Resistance Profile of Serratia Marcescens. Antibiotics 2024, 13, 323, doi:10.3390/antibiotics13040323.
- Zaric, R.Z.; Zaric, M.; Sekulic, M.; Zornic, N.; Nesic, J.; Rosic, V.; Vulovic, T.; Spasic, M.; Vuleta, M.; Jovanovic, J.; et al. Antimicrobial Treatment of Serratia Marcescens Invasive Infections: Systematic Review. Antibiotics 2023, 12, 367, doi:10.3390/antibiotics12020367.
- Abid, S.A.; Al-Kadmy, I.M.S.; Aziz, S.N.; Hamzah, I.H. The Predominance of Virulence Genes Associated with Multidrug-Resistant Serratia Marcescens Isolated from Urinary Tract Infections. Rev. Res. Méd. Microbiol. 2024, 35, 160–166, doi:10.1097/mrm.0000000000000343.
- Tuttobene, M.R.; Gil, B.S.A.; Venanzio, G.D.; Mariscotti, J.F.; Sieira, R.; Feldman, M.F.; Ramirez, M.S.; Véscovi, E.G. Unraveling the Role of UilS, a Urea-Induced Acyl-Homoserine Lactonase That Enhances Serratia Marcescens Fitness, Interbacterial Competition, and Urinary Tract Infection. mBio 2024, 15, e02505-24, doi:10.1128/mbio.02505-24.
- NMESİRİONYE, B.U.; UGWU, C.T.; NWORİE, K.M. Antibiotic Susceptibility and Plasmid Profile of Multidrug Resistant Uropathogenic Serratia Marcescens. J. Microbiol. Infect. Dis. 2022, 12, 12–18, doi:10.5799/jmid.1085914.
- Wang, D.; Haley, E.; Luke, N.; Mathur, M.; Festa, R.; Zhao, X.; Anderson, L.A.; Allison, J.L.; Stebbins, K.L.; Diaz, M.J.; et al. Emerging and Fastidious Uropathogens Were Detected by M-PCR with Similar Prevalence and Cell Density in Catheter and Midstream Voided Urine Indicating the Importance of These Microbes in Causing UTIs. Infect. Drug Resist. 2023, Volume 16, 7775–7795, doi:10.2147/idr.s429990.
- Haley, E.; Luke, N.; Mathur, M.; Festa, R.A.; Wang, J.; Jiang, Y.; Anderson, L.A.; Baunoch, D. The Prevalence and Association of Different Uropathogens Detected by M-PCR with Infection-Associated Urine Biomarkers in Urinary Tract Infections. Res. Rep. Urol. 2024, 16, 19–29, doi:10.2147/rru.s443361.
- Akhlaghpour, M.; Haley, E.; Parnell, L.; Luke, N.; Mathur, M.; Festa, R.A.; Percaccio, M.; Magallon, J.; Remedios-Chan, M.; Rosas, A.; et al. Urine Biomarkers Individually and as a Consensus Model Show High Sensitivity and Specificity for Detecting UTIs. BMC Infect Dis 2024, 24, 153, doi:10.1186/s12879-024-09044-2.
- Parnell, L.K.D.; Luke, N.; Mathur, M.; Festa, R.A.; Haley, E.; Wang, J.; Jiang, Y.; Anderson, L.; Baunoch, D. Elevated UTI Biomarkers in Symptomatic Patients with Urine Microbial Densities of 10,000 CFU/ML Indicate a Lower Threshold for Diagnosing UTIs. MDPI 2023, 13, 1–15, doi:10.3390/diagnostics13162688.
- Kufel, W.D.; Scrimenti, A.; Steele, J.M. A Case of Septic Shock Due to Serratia Marcescens Pyelonephritis and Bacteremia in a Patient Receiving Empagliflozin. J. Pharm. Pr. 2017, 30, 672–675, doi:10.1177/0897190016679760.
- 11. Makusha, L.P.; Young, C.R.; Agarwal, D.R.; Pucar, D. Bilateral End-Organ Endophthalmitis in Setting of Serratia Marcescens Urosepsis on 18F-FDG PET/CT. Clin. Nucl. Med. 2019, 45, e141–e143, doi:10.1097/rlu.0000000000002883.
Dr. Emery Haley is a scientific writing specialist with over ten years of experience in translational cell and molecular biology. As both a former laboratory scientist and an experienced science communicator, Dr. Haley is passionate about making complex research clear, approachable, and relevant. Their work has been published in over 10 papers and focuses on bridging the gap between the lab and real-world patient care to help drive better health outcomes.