C. riegelii
Emery Haley, PhD, Scientific Writing Specialist
Corynebacterium riegelii
Clinical Summary
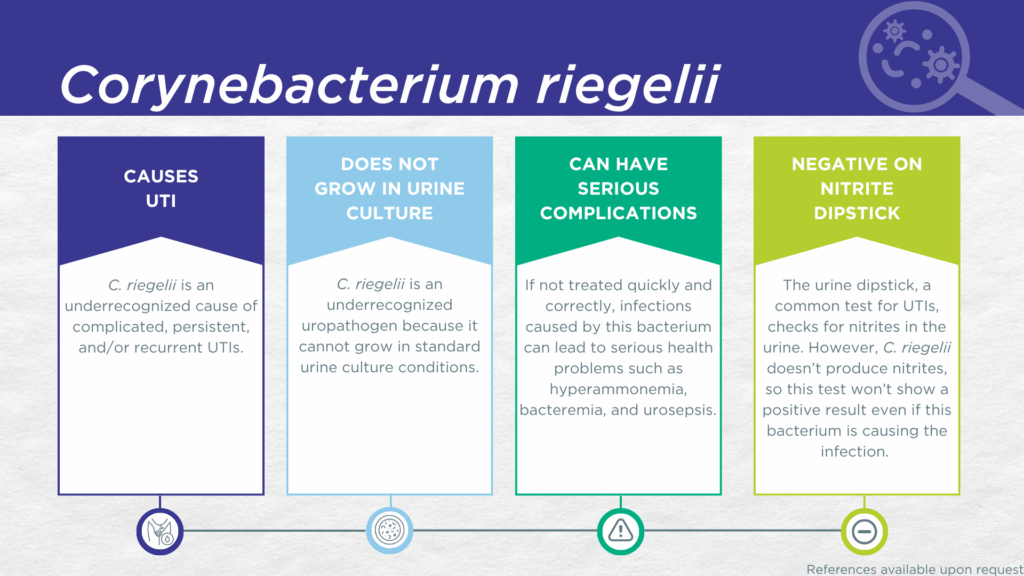
- C. riegelii is a nitrite-negative, urease-positive, gram-positive, microorganism.
- C. riegelii is fastidious and cannot grow in standard urine culture conditions.
- C. riegelii is associated with complicated UTIs.
- In symptomatic UTI patients, C. riegelii:
- Is not a contaminant (is found in catheter-collected urine specimens).
- Is viable (can grow out in expanded culture conditions).
- Is pathogenic (associated with elevated urine biomarkers of infection).
- Reported severe complications of C. riegelii UTI include hyperammonemia, bacteremia, urosepsis, and death.
Bacterial Characteristics
Gram-stain
Gram-positive
Morphology
Bacillus
Growth Requirements
Fastidious (slow growing, prefers blood-agar and 5% CO2)
Microaerophile
Nitrate Reduction
No
Urease
Positive
Biofilm Formation
Unclear
Pathogenicity
Colonizer or Pathobiont
Clinical Relevance in UTI
C. riegelii is a urease-positive microorganism [1]first identified in 1998 by isolation in monoculture with densities > 105 CFU/mL from four female UTI patients with pyuria.[2]
C. riegelii UTIs are likely significantly underdiagnosed due to the numerous challenges in diagnostics. Firstly, C. riegelii lacks nitrate reductase activity, so screening strategies involving urinalysis for nitrite positivity will be false-negative.[1,3] Secondly, in culture, C. riegelii grows preferentially in an anaerobic atmosphere with at least 5% CO2, with particular nutrients (blood agar medium), and needs extended incubation times of at least 48 hours.[2] These conditions are not typically used in clinical laboratories performing standard culture techniques for UTI diagnosis. Thirdly, even when this organism does grow in culture, it is often overgrown by other faster-growing species or dismissed as an irrelevant gram-positive commensal organism of the urogenital microbiome and labeled as a “contaminant”.[4] Instead, C. riegelii UTI is most often diagnosed by advanced proteomic techniques, such as Matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS), or advanced molecular techniques, including polymerase chain reaction (PCR) and sequencing.[4]
A study using expanded quantitative urine culture (EQUC), a technique growing a larger urine volume with additional nutritional media, different atmospheric conditions, and longer incubations, found that the organism was viable.[5] In a study of older adult males and females with clinically suspected complicated UTI, C. riegelii was detected in both midstream voided and in-and-out-catheter collected specimens indicating that it was truly present in the bladder, not simply a contaminant picked up during voiding.[6] Furthermore, elevated markers of immune system activation in the urinary tract have been measured from the same clinical urine specimens in which C. riegelii was detected, indicating that the presence of C. riegelii was associated with an immune response to urinary tract infection.[7–9]
Severe complications of C. riegelii UTI, including hyperammonemia [10] and urosepsis,[11–13] have been reported, with one confirmed death from C. riegelii urosepsis [13].
Together, these findings indicate that C. riegelii should be seriously considered as a uropathogen and demonstrate the value of detecting this organism, particularly in individuals with immune-compromising comorbidities or other risk factors for complicated UTI.
Treatment
Evidence of Efficacy (Checkmarks): Ampicillin, Ampicillin/Sulbactam, Cefepime, Ceftriaxone, Ciprofloxacin, Clindamycin, Doxycycline, Gentamicin, Linezolid, Sulfamethoxazole/Trimethoprim, and Vancomycin.
1. BacDive | The Bacterial Diversity Metadatabase Available online: https://bacdive.dsmz.de/ (accessed on 11 February 2025).
2. Funke, G.; Lawson, P.A.; Collins, M.D. Corynebacterium Riegelii Sp. Nov., an Unusual Species Isolated from Female Patients with Urinary Tract Infections. J Clin Microbiol 1998, 36, 624–627, doi:10.1128/jcm.36.3.624-627.1998.
3. BioCyc Pathway/Genome Database Collection Available online: https://biocyc.org/ (accessed on 11 February 2025).
4. Bernard, K. The Genus Corynebacterium and Other Medically Relevant Coryneform-Like Bacteria. J. Clin. Microbiol. 2012, 50, 3152–3158, doi:10.1128/jcm.00796-12.
5. Festa, R.A.; Luke, N.; Mathur, M.; Parnell, L.; Wang, D.; Zhao, X.; Magallon, J.; Remedios-Chan, M.; Nguyen, J.; Cho, T.; et al. A Test Combining Multiplex-PCR with Pooled Antibiotic Susceptibility Testing Has High Correlation with Expanded Urine Culture for Detection of Live Bacteria in Urine Samples of Suspected UTI Patients. Diagn Microbiol Infect Dis 2023, 107, 116015, doi:10.1016/j.diagmicrobio.2023.116015.
6. Wang, D.; Haley, E.; Luke, N.; Mathur, M.; Festa, R.; Zhao, X.; Anderson, L.A.; Allison, J.L.; Stebbins, K.L.; Diaz, M.J.; et al. Emerging and Fastidious Uropathogens Were Detected by M-PCR with Similar Prevalence and Cell Density in Catheter and Midstream Voided Urine Indicating the Importance of These Microbes in Causing UTIs. Infect. Drug Resist. 2023, Volume 16, 7775–7795, doi:10.2147/idr.s429990.
7. Haley, E.; Luke, N.; Mathur, M.; Festa, R.A.; Wang, J.; Jiang, Y.; Anderson, L.A.; Baunoch, D. The Prevalence and Association of Different Uropathogens Detected by M-PCR with Infection-Associated Urine Biomarkers in Urinary Tract Infections. Res. Rep. Urol. 2024, 16, 19–29, doi:10.2147/rru.s443361.
8. Akhlaghpour, M.; Haley, E.; Parnell, L.; Luke, N.; Mathur, M.; Festa, R.A.; Percaccio, M.; Magallon, J.; Remedios-Chan, M.; Rosas, A.; et al. Urine Biomarkers Individually and as a Consensus Model Show High Sensitivity and Specificity for Detecting UTIs. BMC Infect Dis 2024, 24, 153, doi:10.1186/s12879-024-09044-2.
9. Parnell, L.K.D.; Luke, N.; Mathur, M.; Festa, R.A.; Haley, E.; Wang, J.; Jiang, Y.; Anderson, L.; Baunoch, D. Elevated UTI Biomarkers in Symptomatic Patients with Urine Microbial Densities of 10,000 CFU/ML Indicate a Lower Threshold for Diagnosing UTIs. MDPI 2023, 13, 1–15, doi:10.3390/diagnostics13162688.
10. Yada, K. A Rare Case of Hyperammonemia Caused by Urinary Tract Infection Due to Corynebacterium Riegelii. Cureus 2024, 16, e54082, doi:10.7759/cureus.54082.
11. Matsunami, M.; Matusnami, M.; Otsuka, Y.; Ohkusu, K.; Sogi, M.; Kitazono, H.; Hosokawa, N. Urosepsis Caused by Globicatella Sanguinis and Corynebacterium Riegelii in an Adult: Case Report and Literature Review. J Infect Chemother 2012, 18, 552–554, doi:10.1007/s10156-011-0335-x.
12. Pichon, M.; Micaelo, M.; Longuet, P.; Plantefève, G.; Abderrahmane, M.; Wifaq, B.; Menn, A.-M. A Rare Case of Corynebacterium Riegelii Urosepsis: Role of the MALDI-TOF Mass Spectrometry in the Identification of Emerging Pathogens. Médecine Et Maladies Infect 2019, 49, 474–477, doi:10.1016/j.medmal.2019.06.005.
13. Aygun, G.; Midilli, K.; Cilingir, H.; Yilmaz, M.; Kutukcu, A.; Eker, E. A Fatal Case of Urosepsis Due to Corynebacterium Riegelii. Brazilian Journal of Microbiology 2013, 44, 475–476, doi:10.1590/s1517-83822013000200022.
Dr. Emery Haley is a scientific writing specialist with over ten years of experience in translational cell and molecular biology. As both a former laboratory scientist and an experienced science communicator, Dr. Haley is passionate about making complex research clear, approachable, and relevant. Their work has been published in over 10 papers and focuses on bridging the gap between the lab and real-world patient care to help drive better health outcomes.